Let Me Tell You About Age-Related Macular Degeneration
Let Me Tell You About Age-Related Macular Degeneration
What is Age-Related Macular Degeneration?
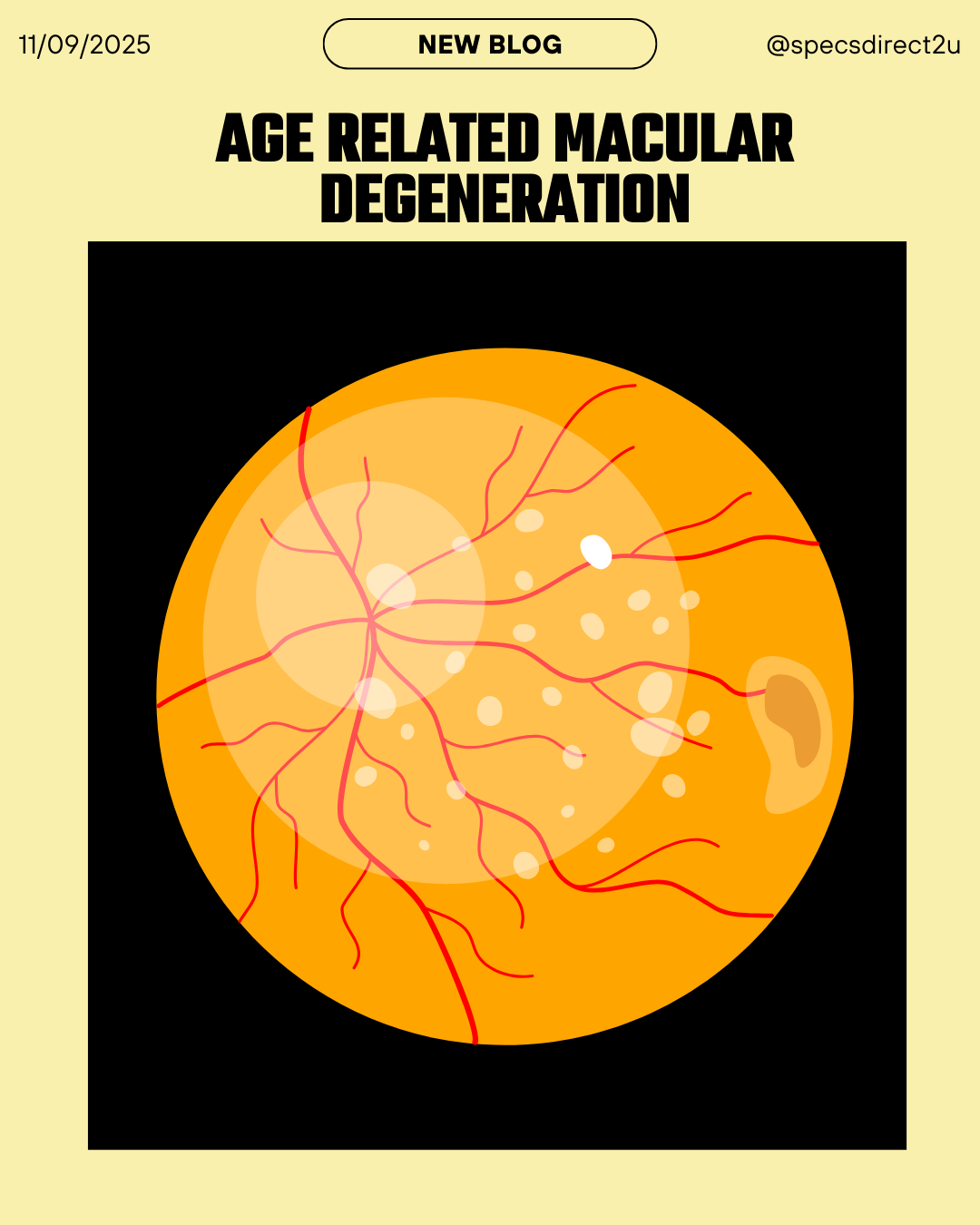
Age Related Macular Degeneration (AMD) is a condition that affects the macula — that’s the central part of the retina in your eye that lets you see fine detail (like reading, recognising faces, watching TV). When the macula is damaged, your central vision gets worse. You may still see things around the edge of your vision (your peripheral vision), but tasks that need seeing straight ahead clearly become harder.
It’s one of the most common causes of sight loss in older people in the UK.

Who Gets It?
- Mostly people over 60, with risk increasing as you get older.
- Not everyone over 60 will get it, many show no signs or only mild signs. But the chance goes up with age. For example, by age 90, there’s about a one in five chance of having AMD.
- Having family members with AMD raises your risk.
Risk Factors
Some things you can’t change; others you can do something about. Here’s the breakdown:
Non-modifiable (can’t change)
- Age: being older is the biggest risk.
- Genetics/family history: If someone close to you has AMD, you’re more likely to develop it.
Modifiable (things you can do something about)
- Smoking: Probably the single biggest lifestyle factor you can change. Smokers have a much higher risk.
- Diet: Eating lots of leafy green vegetables, fruit; getting nutrients is helpful
- Sunlight / UV exposure: Wearing sunglasses that block UV helps reduce risk
- Body weight, blood pressure, and overall cardiovascular health likely have some effect

Types of AMD
There are two main kinds:
- Dry AMD: This is the more common type. In dry AMD, you get build-ups of fatty deposits called drusen, and the macula gradually deteriorates. Vision loss tends to be slow.
- Wet AMD (also called neovascular AMD). Less common, but more serious in terms of how rapidly it can affect vision. New, abnormal blood vessels grow under the macula; they leak fluid or blood, which can damage tissue. Because of that, vision can change quickly.
Also, geographic atrophy is an advanced form of dry AMD, where areas of the retina lose cells permanently

Symptoms & Signs
What might you notice? What will an optometrist or ophthalmologist see?
What you might notice (symptoms)
- Blurred or fuzzy central vision. Things in the centre may look distorted
- Difficulty reading, seeing small print, faces, or fine detail
- Straight lines (door frames, window frames, etc.) may start to look wavy or bent, especially in wet AMD
- Dark or empty patches in the centre of vision
- Colours may seem less bright or more faded
What the clinician sees (signs)
- On eye exam, drusen (yellow deposits) under specific retinal layers
- Changes in retinal pigment, thinning of retina, possibly fluid or bleeding under retina (wet AMD)
- Using imaging tools (OCT – optical coherence tomography) scans can show fluid, swelling, or other structural changes
What to Do If You Think You Have It & When to Seek Help
If you notice any changes in your vision, it’s worth acting quickly.
- Don’t ignore blurry central vision or sudden distortion (e.g., straight lines looking weird). Early detection is particularly important for wet AMD, because treatments work better the earlier they start.
- Use an Amsler chart at home. This is a simple grid of straight lines. If the lines look wavy, missing, or distorted, that could be a signal to go to an optometrist. Many eye clinics or organisations provide these charts.
- Go for regular eye examinations (optometrist), especially once you’re over 60 or have other risk factors. Even if vision seems okay, optometrists can spot early signs.
- If you have dry AMD, keep an eye on changes; if you have signs of wet AMD (sudden distortion or rapid worsening), get urgent help. Wet AMD needs prompt treatment
Treatments & What Can Help
While there’s no cure yet for all forms of AMD, there are ways to slow progression, manage symptoms, and, for wet AMD, treat more aggressively.
For Dry AMD
- Currently, no treatment reverses dry AMD or restores macula cells that are lost. The approach is to slow progression and preserve vision.
- Lifestyle changes: stop smoking, wear UV-protective sunglasses, eat well, and keep cardiovascular health good.
For Wet AMD
- There are treatments using anti-VEGF injections (drugs injected into the eye), which slow down or stop the growth of abnormal blood vessels. These can reduce further damage
- You’ll probably need regular monitoring (every month or every few weeks) at hospital eye clinics, along with scans to see how the disease is progressing

Vitamins / Diet / AREDS
Since many people ask about vitamins: here’s what the evidence shows, especially from the AREDS / AREDS2 studies (Age-Related Eye Disease Studies) and related guidance.
- The AREDS and AREDS2 trials showed that certain combinations of antioxidant vitamins and minerals can reduce the risk of progression from intermediate AMD to advanced AMD in people who already have some AMD.
- But vitamins/mineral supplements do not appear to prevent the initial onset of AMD in people who don’t already have it. There is currently no evidence to such this.
- Leafy green vegetables (spinach, kale, broccoli, etc.) are good sources of natural nutrients like lutein and zeaxanthin, which are protective. Fruit, a varied diet helps
Signs When AMD Is Worsening
It’s especially important to act when:
- Distortion appears (straight lines look curved), or you notice a rapid change in vision.
- Blind or dark patches in the centre develop quickly.
- If the disease is in one eye and seems stable, but then you notice symptoms in the other eye.
Summary & Takeaway
- AMD is common, especially in older adults; it affects central vision.
- There are dry and wet types; wet is less common but more aggressive.
- You can’t change your age or genetics, but lifestyle matters: don’t smoke, protect your eyes from UV, and eat well.
- Vitamins and minerals (AREDS / AREDS2 formula) can help if you already have intermediate-AMD, to slow progression.
- An Amsler chart and regular eye checks are good ‘early warning’ tools.
- Seek help from an optometrist or eye clinic if you notice changes — especially sudden changes.
Below you will find an amsler chart and some more information provided by the Association of Optometrists: